|
Christmas Message From Our CEO, Carolyn Donohoe
As we approach the Christmas season, I want to extend my heartfelt thanks to every nurse and midwife across Ireland for your extraordinary commitment throughout the year. Your professionalism, compassion and resilience continue to shape the highest standards of care in our health system.
This time of year, offers a moment to pause and appreciate the collective effort that strengthens our professions and support the public we serve.
As I reflect on 2025, I am filled with a profound sense of pride and optimism. This year has been one of steady progress, marked by significant achievements in public protection, professional development and strategic innovation.
As we approach the Christmas season, I want to extend my heartfelt thanks to every nurse and midwife across Ireland for your extraordinary commitment throughout the year. Your professionalism, compassion and resilience continue to shape the highest standards of care in our health system.
This time of year, offers a moment to pause and appreciate the collective effort that strengthens our professions and support the public we serve.
As I reflect on 2025, I am filled with a profound sense of pride and optimism. This year has been one of steady progress, marked by significant achievements in public protection, professional development and strategic innovation.
Education and standards development
One of the most significant milestones of 2025 was the launch of the updated Code of Professional Conduct and Ethics for Registered Nurses and Registered Midwives in February.
This new Code reflects the evolving realities of modern healthcare, strengthens the principles that underpin safe and ethical practice and provides clearer guidance for registrants. The launch marked a major step forward in supporting professional judgement, enhancing public trust and guiding practice for years to come. Its development was shaped by extensive consultation with nurses, midwives, educators, employers and members of the public ensuring it truly reflects the values and expectations of those we serve.
We collaborated closely with education partners to update the undergraduate pre-registration standards and requirements for nursing and midwifery programmes. The revised edition will reform entry to the Register standards for future graduates to ensure they equipped with the skills and competencies needed in an evolving health environment.
Our pilot of the Professional Competence Scheme continued in healthcare sites across the country. The pilot represents an important step toward supporting ongoing professional development for nurses and midwives. Working closely with pilot sites, we have been evaluating practical models for maintaining competence and the insights gained will inform the design of a future scheme that promotes lifelong learning, enhances professional accountability and strengthens public confidence in the professions.
Registration and digital transformation
The hard work of our Registration Department has been clear this year and one of the highlights of 2025 has been the continued expansion of our Register, reflecting the vital role nurses and midwives play in Ireland's healthcare system. Our annual State of the Register 2025 report, published in November, reveals a robust picture and as of 1 June 2025, there were 92,385 registrants, a 3% increase from the previous year and the highest number of nurses and midwives on our Register.
We welcomed 1,649 newly qualified Irish-educated nurses and midwives to the Register and also welcomed 3,487 internationally educated professionals. These figures are more than numbers; they represent a workforce equipped to meet Ireland's healthcare demands.
Our Digitisation team have also done incredible work, successfully launching our enhanced MyNMBI portal. The digital portal for registrants, applicants and education bodies has been streamlined to deliver faster, more intuitive services, and improve the registration and annual renewal processes. I am immensely proud of what the team have achieved.
Strengthening regulation and public protection
Public protection is our core imperative and this year, we continued to modernise our regulatory frameworks to ensure they remain strong, transparent and responsive to the needs of the public and the professions. Key improvements to our Fitness to Practise processes helped streamline timelines, enhance communication, and support all participants with greater clarity and consistency.
Building on our upstream regulation focus, we continued our work to provide compassionate support for anyone involved in the FTP process. In 2025, NMBI placed a strong emphasis on strengthening the supports available to individuals involved in the fitness to practise process. Recognising the personal and professional impact that participation in a regulatory process can have, we advanced several initiatives to ensure that all witnesses are treated with dignity, clarity and compassion.
These developments reflect our ongoing commitment to ensuring that the fitness to practise process is fair, transparent and sensitive to the needs of all participants, while maintaining the integrity of the regulatory system and the central objective of protecting the public.
Fostering engagement and partnerships
Throughout 2025, we deepened engagement with our registrants and stakeholders. Through consultations, forums and events, we ensured that the voices of nurses and midwives remain central to regulatory development.
It is with genuine gratitude and deep respect that I mark the end of Dr Louise Kavanagh McBride’s term of office as NMBI President.
Louise has provided exceptional leadership and has led with calm authority and an unwavering focus on public safety. Her ability to balance progressive reform with the highest standards of governance has been remarkable. Equally importantly, she has been an outstanding advocate for our registrants, consistently highlighting their skill, dedication and central role in Ireland’s health service.
On a personal note, it has been a privilege to work alongside Louise. Her support has been invaluable and the culture of collaboration she has fostered across the organisation will endure long after her presidency ends.
From all at NMBI, we wish her continued success in the future.
I would also like to extend my congratulations to Áine Lynch who was recently elected as our new President and I look forward to working with her as she guides the organisation through the next phase of development.
Finally, I would like to extend my deepest thanks to every nurse, midwife, educator, employer and all our stakeholders whose passion fuels our work. Together, we have not only regulated but elevated our professions, ensuring safe, compassionate care.
From all at NMBI, we wish you a very happy Christmas and a prosperous New Year filled with health, fulfilment and renewed energy.
Thanks,
Carolyn
|
|
NMBI Extends its Thanks to our President as her Term of Office Ends
As our President, Dr Kavanagh McBride’s term of office comes to a close, we reflect on a period of significant progress under her leadership.

As our President, Dr Kavanagh McBride’s term of office comes to a close, we reflect on a period of significant progress under her leadership. Her tenure has been marked by vision, collaboration, and a deep commitment to advancing nursing and midwifery standards for the benefit of patients and the public.
Louise’s journey into nursing began at the Mater Misericordiae Hospital in Dublin, where she trained as a general nurse before specialising in Orthopaedics and Emergency Nursing. Her passion for education and professional development led her to pursue an MSc in Nursing Science, a PhD, and numerous postgraduate qualifications, including a Fellowship of the NMRCSI and diplomas in Clinical Health Science Education, Psychology and Management.
Today, she serves as Head of the Department of Nursing & Healthcare at Atlantic Technological University (ATU) Donegal, where she is principal investigator/partner/mentor on several Irish and European research funded projects in mental health and wellbeing for college students and Digital Healthcare solutions. Her academic leadership reflects a deep commitment to preparing future generations of nurses and midwives for an evolving healthcare environment.
Louise joined the NMBI Board in 2015 as the Technological Higher Education Association representative and served as Vice-President from 2017 to 2023. During her presidency, she has championed the implementation of NMBI’s Statement of Strategy 2023–2025, focusing on education, training and standards while ensuring public protection remains at the heart of the organisation’s work.
Her leadership has enhanced partnerships across healthcare regulation and she leaves a legacy of integrity, compassion and collaboration. Her work has strengthened NMBI’s role as a regulator and championed the professions, ensuring that the NMBI is well-positioned to meet future challenges and opportunities.
As her term concludes, our CEO, Carolyn Donohoe said: "Louise leaves behind more than achievements; she leaves a legacy of mentorship and reflection. Her story reminds us that leadership in healthcare is not just about governance; it is about people, values and the belief that care can transform lives".
We would like to extend our thanks and best wishes to Louise. She will be greatly missed within the organisation and by our colleagues and stakeholders.
NMBI Announces New Board President
NMBI has announced the election of Áine Lynch as its new Board President following a Board meeting on 24 November 2025. Áine takes-up office in January 2026.
NMBI has announced the election of Áine Lynch as its new Board President following a Board meeting on 24 November 2025. Áine takes-up office in January 2026.
Áine was appointed a board member of NMBI by the Minister of Health in 2021, nominated by the Health Service Executive (Directors of Nursing or Directors of Midwifery) and was elected Vice-President in 2023.
She has over 40 years’ experience in healthcare across Ireland, the UK and the Middle East. Áine spent many years in several different roles at Tallaght University Hospital including Ward Manager, Clinical Facilitator and Assistant Director of Nursing, Nurse Practice Development. She has been Director of Nursing & Integrated Care at Tallaght University Hospital since 2017 where she leads a team of over 1,600 registered general nurses and 250 Health Care Assistants. Other areas of responsibility include the Integrated Care brief, Patient Advice and Liaison Service, Pastoral Care team and the Arts and Health Department. She is the executive lead for the Patient Community Advisory Council.
Áine worked at regional level in 2016-2017 as Interim Director of the Nursing and Midwifery Planning and Development Unit, Dublin South Kildare & Wicklow, Office of the Nursing & Midwifery Services Director, HSE. In 2022-2023 she undertook the role of interim Chief Director of Nursing and Midwifery, Dublin Midlands Hospital Group.
She is an Adjunct Associate Professor, School of Nursing & Midwifery, Trinity College Dublin, awarded in 2018. In 2023, Áine was awarded Fellow by Examination, Nursing and Midwifery, Royal College Surgeons in Ireland.
Speaking on her appointment, Áine Lynch said: “It is an honour and privilege to have been elected President of NMBI and l would like to thank my Board colleagues for their trust in electing me. I would also like to pay special tribute to our outgoing President, Dr Louise Kavanagh McBride, for her guidance and leadership over the last three years.
“As I move from Vice-President into this new role, I am acutely aware of the opportunities and challenges ahead for nursing and midwifery. I look forward to working collaboratively with the Board, the executive team and our key partners as we continue our important work to support and empower the professions of nursing and midwifery.”
Congratulating Áine Lynch on her election, Carolyn Donohoe, NMBI Chief Executive Officer said: “Áine Lynch’s proven leadership and deep commitment to the professions of nursing and midwifery puts NMBI in a strong position for the years ahead. As we congratulate our new President on her appointment, I would also like to recognise our outgoing President, Dr Louise Kavanagh McBride, whose leadership has made a lasting impact on our organisation.”
|
|
Christmas/New Year Opening Hours for Annual Renewal Assistance
We would like to advise registrants who are completing their annual renewal of our Christmas and New Year opening hours.
We would like to advise registrants who are completing their annual renewal of our Christmas and New Year opening hours.
The 2026 annual registration renewal window is open until 31 January 2026. To date more than 40,000 nurses and midwives have renewed their registration and we would like to thank them for completing the process. For registrants who have yet to renew, we would advise them to login as soon as possible to avoid peak times later this month.
Anyone who is having difficulties logging in or renewing online, can contact our customer care team on 0818 200 116 (+353 818 200 116 from outside Ireland) or by email at regservices@nmbi.ie. When contacting us, please provide your name, PIN number and your date of birth as this will help us deal with any query more efficiently.
Our opening times over this period can be found below.

The annual renewal process must be completed through our online portal, MyNMBI. We cannot accept annual renewal payments by phone. The portal was recently upgraded to ensure the renewal process is as user-friendly as possible. While the portal may look different, the process is the same and will only take a few minutes to complete. Your username has not changed; however, you will need to change your password to access your account.
We have developed several useful guides to assist registrants through the process. They can be found on our website.
Registrants can voluntarily remove their name from the Register of Nurses and Midwives on MyNMBI, free of charge until 31 January 2026. We highly recommend that you voluntarily remove your name from the Register rather than let your registration lapse (that is, not renew your registration on time). This will ensure that you will avoid paying increased restoration fees in the future. More information about the voluntarily removal process can be found on our website.
The annual registration renewal goes towards our work to support nurses and midwives to provide the highest standards of professional practice. Through our registration, education and guidance, and fitness to practise functions we enhance the safety of service users. Further information about the work we do can be found on our website.
|
|
Second Student Nurse Ambassador Forum Held
On 27 November, we held the second Student Nurse Ambassador Forum at our Office in Blackrock, Dublin.

On 27 November, we held the second Student Nurse Ambassador Forum.
Speaking at the opening of the Forum, NMBI President Dr Louise Kavanagh McBride said: "Our Student Nurse Ambassadors are a voice for our student community. Their input and engagement will raise the profile of students as valued members of the profession, while their commitment will inspire those considering a career in nursing to take that first step on the path.”
The event is a unique opportunity for undergraduate nursing students to meet with NMBI and understand the role of their regulator in supporting them throughout their careers. The Student Ambassadors will partner with NMBI in promoting the profession, as well as participate in NMBI events throughout the year.

Twenty student nurses from the four primary nursing divisions, General Nursing; General and Children’s Nursing; Mental Health Nursing and Intellectual Disability Nursing, attended the forum from the higher education institutions.
NMBI Chief Executive Officer, Carolyn Donohoe said: “By building this connection, we believe our Student Nurse Ambassadors will use the forum as a platform to shape their futures – we want to hear their voices and embrace their vision for the future, as they embark on their careers.”
Other speakers included Lorraine Clarke Bishop, Interim Director of Education, Policy, Standards; Dr Ray Healy, Director of Registration; Yvanne Kennedy, Interim Director of Fitness to Practise and Kathyann Barrett, Head of Operations.

Picture above (L to R): Lorraine Clarke Bishop, Dr Louise Kavanagh McBride and Carolyn Donohoe
The students participated in a series of round table discussions on topics such as why they decided to become a nurse and the priorities for student nurses and new graduates.
Colleagues from Pflegekammer Nordrhein-Westfalen, a German regulator, joined virtually to share insights into their student ambassador programme.
Bringing proceedings to a close, Lorraine Clarke Bishop, Interim Director of Education, Policy, Standards said: “This event serves to strengthen the connection between NMBI as the regulator and student nurses. We believe this partnership will inspire and empower students to play an active role in contributing to the advancement of the profession.”
Decision Following Fitness to Practise Inquiry
The Board of NMBI has published the outcome of a complaint following the fitness to practise process.
The Board of NMBI has published the outcome of a complaint following the fitness to practise process.
The finding is published on NMBI's Findings and Decisions page.
|
|
Meet our Student Nurse Ambassadors
|
Children’s and General Nursing
|
|

|
Michelle Burford
3rd Year
Trinity College Dublin
|
|
General Nursing
|
|

|
Áine Marie McBride
3rd Year
Atlantic Technological University Donegal
|
|

|
Annabel Whitty
3rd Year
South East Technological University
|
|

|
Ava Casey
3rd Year
South East Technological University
|
|

|
Brian Rusk
3rd Year
University College Dublin
|
|

|
Ella Scannell
3rd Year
Technological University of the Shannon
|
|

|
Emma Glennon
3rd Year
University of Galway
|
|

|
Isabela Estrela
3rd Year
Technological University of the Shannon
|
|

|
Killian Spain
2nd Year
University of Limerick
|
|

|
Rigina Kelly
3rd Year
Atlantic Technological University St Angela’s Sligo
|
|

|
Zuzanna Wesolowska
3rd Year
Atlantic Technological University Donegal
|
|
Intellectual Disability Nursing
|
|

|
Charis Tomb
2nd Year
Dublin City University
|
|

|
Saoirse Hayes
3rd Year
Atlantic Technological University St Angela’s Sligo
|
|

|
Senzeni Mpofu
4th Year
University College Cork
|
|
Mental Health Nursing
|
|

|
Ayush Rigal
2nd Year
University College Dublin
|
|

|
John McQuaid
3rd Year
Dundalk Institute of Technology
|
|

|
Megan Kiely
4th Year
University of Limerick
|
|

|
Modesta Dunauskaite
3rd Year
Dundalk Institute of Technology
|
|

|
Poppy Wynne
2nd Year
University of Galway
|
|

|
Kimberly Chafa
1st Year
Trinity College Dublin
|
Spotlight On: Enhancing the Patient Journey Through Intensive Care Services
The Critical Care ANP Team, St James’s Hospital, Dublin
As the largest cohort of healthcare employees, nurses play a pivotal role in global healthcare reform. In March 2020, the Critical Care Advanced Nurse Practitioner (CCANP) service was developed by a team of Advanced Nurse Practitioners (ANP) at St James’s Hospital (SJH), Dublin.

The Critical Care ANP Team, St James’s Hospital, Dublin
As the largest cohort of healthcare employees, nurses play a pivotal role in global healthcare reform. In March 2020, the Critical Care Advanced Nurse Practitioner (CCANP) service was developed by a team of Advanced Nurse Practitioners (ANP) at St James’s Hospital (SJH), Dublin. The service was established in response to the Irish Government’s Critical Care Strategic Plan. The aim of this plan is to increase critical care bed capacity, to target the under provision of intensive care unit beds and meet the national key performance indicators related to admission targets for critically ill patients.
The CCANP team in St James’s Hospital is just one of approximately 43 specialities and subspeciality ANP services available at the hospital. Comprised of eight experienced intensive care nurses, the CCANP team strive to make a meaningful difference to the deteriorating critically ill patient throughout the hospital.
The CCANP team, are purpose driven and results focused, with a commitment to advancing nursing, strengthening staff capability, promoting nurse research and leadership, and pursuing excellence in patient outcomes.
Our ANP service is divided into a four-pillar approach underpinned by research and audit. The pillars consist of patient care in pre-ICU, in ICU and post-ICU, with education provision allowing for the empowerment of both patients and hospital staff. This approach ensures CCANPs involvement in patient care from the moment of deterioration to discharge from ICU and includes attendance at the ICU recovery clinic from home.
The fundamental premise is that to achieve optimal patient outcomes and nurse satisfaction, nurse competencies must be driven by patient and service need in alignment with the HSE (2014) vision of ICU without walls, ensuring the ‘right patient, is with the right people, in the right place, at the right time’.
Admitting patients to the ICU as quickly as possible is crucial because delayed admission to critical care is strongly associated with increased morbidity, higher mortality rates and longer hospital stays.
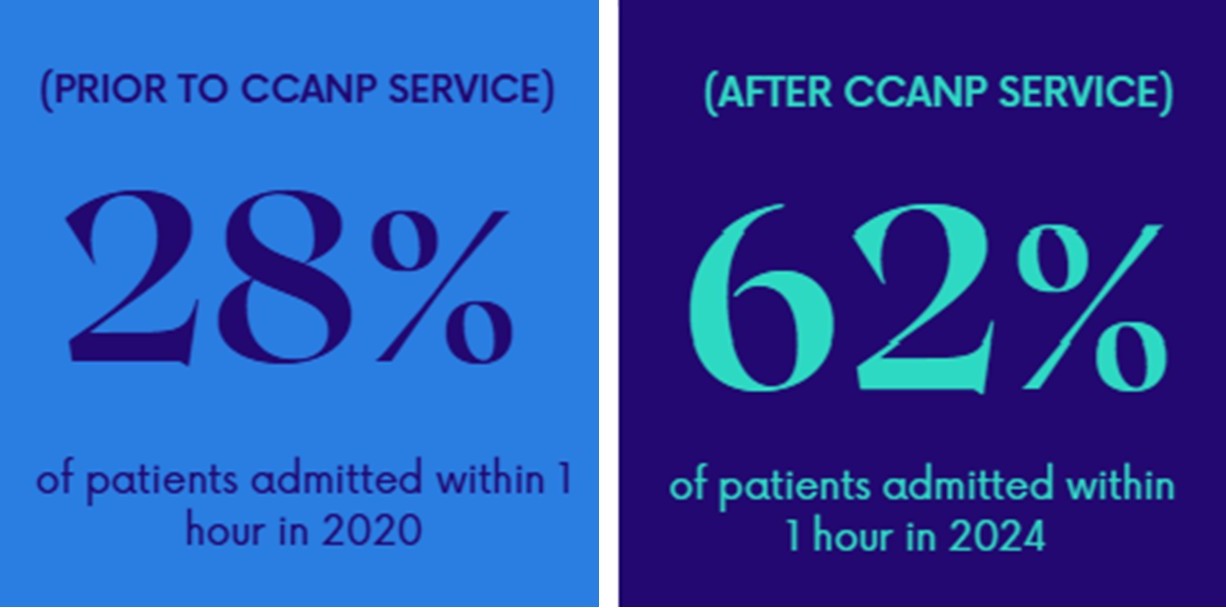
The CCANP team’s admission Key Performance Indicator targets for critically ill patients are benchmarked against the National Office of Clinical Audit data, 2023: 50% of patients should be admitted within one hour of the decision to admit and 80% of patients should be admitted within four hours of the decision to admit.
In partnership with nursing, medical and multidisciplinary colleagues, and with the provision of the emergency bed, the CCANP team have superseded these admission targets. In 2024, the CCANP service facilitated 50% of unplanned admissions. 62% were admitted within one hour and 99% were admitted within four hours.
Once a decision has been made to admit the patient, a member of the CCANP team is immediately available to manage the deteriorating patient on the ward and facilitate enroute procedures. When enroute procedures or investigations are taken into consideration, 85% of patients were admitted within one hour. This is important to note, as we are patient focused, not KPI driven. It is more important for this cohort of patients to receive efficient prognostication than to be expediated to the ICU.
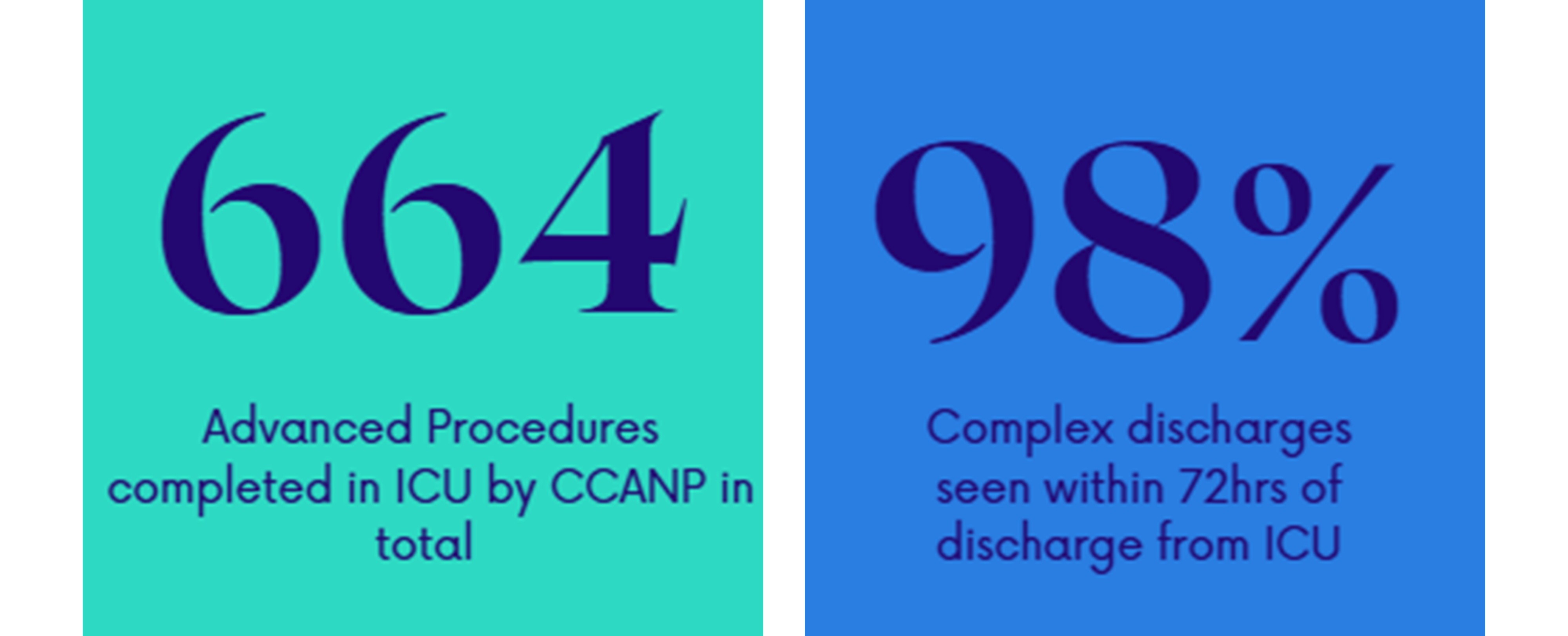
Enhancing the patient journey throughout ICU, the CCANP team lead manages a patient’s caseload and performs several advanced procedures. In 2024, 1,132 patients were reviewed by the CCANP team within the ICU and 664 advanced procedures were carried out including: arterial lines, male catheterisations, ultrasound guided vascular access and NG tubes.
The team also lead on several quality improvement (QI) initiatives. One of these is the ANP-led PICC line insertions service. This service means that patients can have specialised long term vascular access placed at their bedside in a timely manner without the need for transfer to the Interventional Radiology Department.
Another QI initiative the team are proud to lead on is the Antibiotic Allergy DE-labelling in ICU (ADE-ICU). Critically ill patients in ICU are frequently prescribed antibiotics, with many reporting an antibiotic allergy label, predominantly to penicillin. Mislabelling contributes to suboptimal antibiotic use, increasing multidrug-resistant organisms and Clostridium difficile infections, and increased hospital length of stay. Removing inaccurate labels decreases the risk of hospital acquired infections, e.g. MRSA, VRE, MDR-GNB, C. difficile and reduces hospital/ICU length of stay.
The ANP service in St James's Hospital aims to optimise the care and transition of the critically ill adult to and from the ICU. Recovery after critical illness can be a challenging journey for patients and their care providers. The transition from critical care to ward-level care is the first step in this journey, and patients are vulnerable to clinical deterioration and psychological distress.
The CCANP service aims to reduce errors, ease distress, identify risk of Post Intensive Care Syndrome (PICS) and optimise transition of care of the patient. In 2021, a traffic light system was developed by the CCANP and ICU consultant team to determine the necessity of post ICU review of patients on the ward. Red category patients were to be seen in-person, Amber category were reviewed at CCANP discretion and from Q4 2022, Green patients were reviewed remotely to identify TOC issues.
Another focus of our ICU stepdown reviews is to identify and support patients at risk of PICS. In 2024, 839 patients were followed up the team, 98% of all discharges from ICU. Over 70% of our patients are now surviving ICU, but survival often comes at a cost.

PICS is a relatively new concept which describes the sometimes-catastrophic impact of ICU survivorship on both patients and their families (PICS-F). PICS is made up of health problems that remains after critical illness. This led to the foundation of the ANP-led ICU Recovery Clinic. The ICU Recovery Clinic plays a pivotal role enabling patients and their families to understand their ICU journey and effectively manage symptoms of PICS. We hope that with this continued support from the CCANPs, our patients will not only survive but thrive as they adjust to life post-critical illness.
10-16 November marked International Advanced Nurse Practitioner Week. The theme of this year’s celebrations was “Trusted Voices, Proven Care”, and with over 1,380 ANPs nationwide, advanced practice nursing continues to play an integral and dynamic part in improving patient outcomes and the patient care experience. ANPs offer a valuable and cost-effective resource to address the challenges of accessible, safe and affordable health care.
The success of the CCANP role is in part attributable to and contingent on, the continued support of frontline staff nurses, Clinical Nurse Managers, Clinical Facilitators, medics and the wider multidisciplinary team across health and social care.
|
|
|