The Board of the NMBI has 23 members with a lay majority of 12. Of the remaining 11 members, eight are registered nurses and midwives elected by the professions. A further three nurses and midwives are appointed by the Minister for Health.
In order to ensure continuity, not all Board members’ terms of office end at the same time. Of the 23 Board members, the terms of office of 11 members ended on 5 December 2020. Two of those members were reappointed by the Minister for Health:
- Louise Kavanagh McBride – nominated for appointment by the institutes of technology
- Laura Sahm – nominated for appointment third level education
The following six members were appointed by the Minister for Health:
- Áine Lynch – nominated by directors of nursing and midwifery
- Siobhán McArdle – nominated for appointment by the HSE
- Louise Collins – nominated for appointment by the HSE
- Conan McKenna – appointed to represent the public interest
- Anne Marie Duffy – appointed to represent the public interest
- Cyril Sullivan – appointed to represent the public interest
In addition, an election was held in September 2020 in three categories with the successful candidates being appointed to the Board by the Minister in January 2021:
- Lorraine Clarke-Bishop – re-elected in the nursing/midwifery education category
- Joseph Shalbin – elected in the general nurse category
- Marian Vaughan – elected in the children’s nurse category
The terms of office of the remaining 12 members will end on 5 December 2022.
Below are profiles of the eight new members of the Board:
Áine Lynch
 Áine is a registered general nurse for more than 33 years and has spent her career predominantly in the acute hospital setting in Dublin following a number of years in the UK and Saudi Arabia.
Áine is a registered general nurse for more than 33 years and has spent her career predominantly in the acute hospital setting in Dublin following a number of years in the UK and Saudi Arabia.
From 1998 she has enjoyed several roles in Tallaght University Hospital (TUH) including Clinical Nurse Manager 2 in Trauma Orthopaedics, Clinical Facilitator in Orthopaedic Nursing, Nurse Practice Development Advisor CNM 3 and Assistant Director of Nursing, Nurse Practice Development Department.
In 2016 she moved from TUH to the Nursing and Midwifery Planning and Development Unit (NMPDU) Dublin, South Kildare and Wicklow where she initially worked as Nursing and Midwifery Planning and Development Officer and later held the role of Interim Director.
Áine returned to TUH in April 2017 as Director of Nursing. Along with leading the nursing service of more than 1,000 Registered Nurses and Health Care Assistants, she is executive lead for the Patient Advice and Liaison Service, Pastoral Care Department, End of Life Care, and the Arts and Health team. She acts as executive lead for the Patient and Community Advisory Council and has assumed the role of Executive Integrated Care Lead in November 2020.
In the earlier part of her career Áine completed the English Nursing Board 2019 Orthopaedic Nursing programme, a Bachelor of Nursing Science (TCD) and a Master’s in Education and Training (DCU). In 2019 she completed a Diploma in Leadership Development in the UCD Michael Smurfit Graduate Business School. She is currently undertaking an Executive Leadership programme for Directors of Nursing and Midwifery through the National Leadership Centre for Nursing and Midwifery, ONMSD, and the RSCI Institute of Leadership. She holds the position of Adjunct Associate Professor in the School of Nursing and Midwifery, Trinity College Dublin.
Anne Marie Duffy
 Anne Marie is an independent expert on curriculum, assessment and regulation participating in a range of projects both local and within European states. She is a Non-Executive Director on the regulatory body ‘Qualifications Wales’. She serves on the governing bodies of a number of charities.
Anne Marie is an independent expert on curriculum, assessment and regulation participating in a range of projects both local and within European states. She is a Non-Executive Director on the regulatory body ‘Qualifications Wales’. She serves on the governing bodies of a number of charities.
Anne Marie holds a BA (Hons) and Master’s Degree in Education from Queens University Belfast. She is an alumnus of the Chief Executive’s Forum Women’s Leadership Programme. She was appointed OBE in 2017 for Services to Education. Anne Marie held the role of Director of Qualifications and Responsible Officer within CCEA (Council for Curriculum, Examinations and Assessment) directing the design, operation and grading of public examinations.
She was a member of the Chief Executives’ Forum of the Joint Council for Qualifications (UK) and held the role of non- Executive Chair of the Qualifications Governance Council of NEBOSH (National Examinations Body for Occupational Safety and Health). Anne Marie has more than 36 years of experience working within the public sector, latterly within the highly regulated area of public examinations, complying with regulatory conditions across England, Wales and Northern Ireland.
She now serves on the Regulatory Board of Qualifications Wales and thus brings to NMBI experience of working on both sides of regulation. As Director of Qualifications within CCEA, Anne Marie led and directed CCEA’s digital transformation programme with the onscreen marking project gaining a UK NextGen award for public sector transformation in 2017. She brings significant experience in change management and stakeholder engagement to NMBI. Responsible also for leading investigations into allegations of malpractice, Anne Marie brings to the Board expertise in governance, accountability and evidence-based decision making.
Dr Conan McKenna
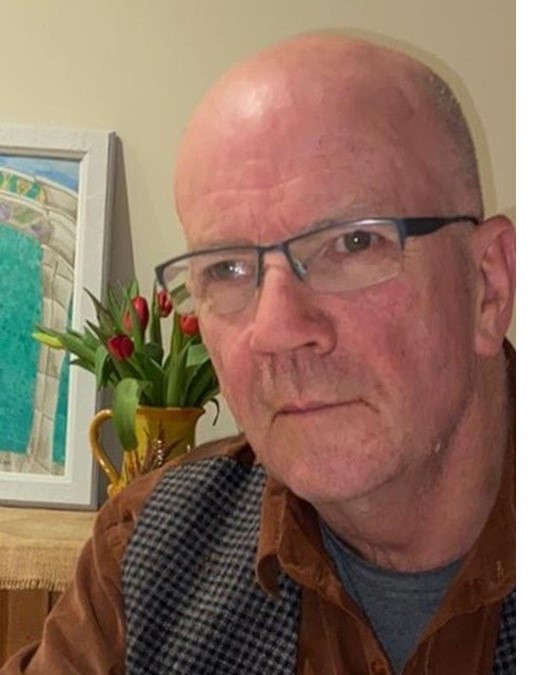 Conan is a part-time management consultant and lecturer at the Institute of Public Administration in areas including Human Resources Management, Organisation Behaviour and Strategy. He also chairs the Audit and Risk Committee of the Data Protection Commission and is a member of the Complaints Committee of the Legal Services Regulatory Authority.
Conan is a part-time management consultant and lecturer at the Institute of Public Administration in areas including Human Resources Management, Organisation Behaviour and Strategy. He also chairs the Audit and Risk Committee of the Data Protection Commission and is a member of the Complaints Committee of the Legal Services Regulatory Authority.
He retired in recent years from full time work as an assistant secretary general in the Department of Justice and Equality where he was responsible for policy in relation to the Courts and was a member of the Board of the Courts Service. He was also responsible for policy and key legislative reforms in relation to regulation, family law (including the 2015 Marriage Equality Referendum), assisted decision making, civil liability/medical negligence and the legal professions. Conan also worked as part of the senior management team in the Houses of the Oireachtas over many years, developing expertise in senior leadership of Financial, ICT, Human Resources and change management/governance. During this period, he also developed considerable expertise and experience in relation to parliamentary committees and inquiry work as well as associated legal matters.
During his public sector career of more than 40 years, he worked across seven different organisations. Conan originally graduated from UCD with a degree in English and subsequently qualified as a barrister at law. He also studied Management Information Systems at the Irish Management Institute and has an MSc in Management (Organisation Behaviour/HR) from TCD and a Doctorate in Governance from Queens University, Belfast.
Conan is delighted to have been appointed to the Board and sees this as an opportunity to learn about a sector completely new to him and, at the same time, apply his experience and expertise to helping NMBI in whatever ways he can to manage key challenges and deliver on its strategies and ambitions in the coming years.
Dr Cyril Sullivan
 Cyril is a qualified accountant (FCCA/ACMA) with more than 30 years’ experience in the profession. Dr Sullivan is currently the Director/ Chief Officer with ECC Ireland and he has held a number of senior executive positions in the public sector including Director of Finance and Support Services with the Institute of Public Administration (IPA), Head of Finance and Corporate affairs with the National Roads Authority (NRA) and an auditor with the Comptroller and Auditor General’s (C&AG) Office.
Cyril is a qualified accountant (FCCA/ACMA) with more than 30 years’ experience in the profession. Dr Sullivan is currently the Director/ Chief Officer with ECC Ireland and he has held a number of senior executive positions in the public sector including Director of Finance and Support Services with the Institute of Public Administration (IPA), Head of Finance and Corporate affairs with the National Roads Authority (NRA) and an auditor with the Comptroller and Auditor General’s (C&AG) Office.
Cyril has had a number of State nominations including being a member of the Audit Committees of the Department of Health and Department of Community, Rural and Gaeltacht Affairs and he is currently on his second term as a member of the Audit Committee of the Department of Children, Equality, Disability, Integration and Youth and with the Citizens Information Board. Cyril has just finished his second term as Chair of the Audit and Risk Committee of An Garda Siochana.
His expertise is in the areas of governance, financial management, ICT, audit and risk. As well as being a qualified accountant, Cyril has a B.Sc in Computer Science (TCD), an M (Econ) Sc in Policy Studies (TCD), an MBA (Smurfit Business School, UCD) and a Doctorate in Governance (Queens University, Belfast).
Joseph Shalbin Kallarakkal
 Joseph was elected to the Board in last year’s election in Category A as a registered nurse from the practice of general nursing engaged in clinical practice.
Joseph was elected to the Board in last year’s election in Category A as a registered nurse from the practice of general nursing engaged in clinical practice.
A Registered General Nurse, Joseph had been working in St. James’s Hospital, Dublin but recently joined the staff in Our Lady’s Hospital, Navan. Apart from his nursing qualifications, he has a Bachelor’s Degree in Commerce and a MBA in Healthcare Service Management. He is a vice-chairperson in the INMO’s International Section.
As a union representative Joseph successfully argued in 2019 for nurses/midwives from overseas should be recognised as Critical Workers.
Louise Collins
 Louise is Director of Clinical Services (Health and Social Care Professions) in Connolly Hospital, Blanchardstown.
Louise is Director of Clinical Services (Health and Social Care Professions) in Connolly Hospital, Blanchardstown.
She qualified as a Speech and Language Therapist with a BSc. (Hons) Speech Sciences from University College London (UCL) in 1992 and worked in community and rehabilitation services in the NHS until 2000. On her return to Ireland, she worked in acute services (Mater Misericordiae University Hospital) and as Speech and Language Therapy Manager in Connolly Hospital. Her clinical expertise lies in care of the older person, stroke and mental health services.
Louise has been a member of the executive management team at Connolly since 2013 undertaking roles in operations as well as health and social care professions lead.
Her academic qualifications include a Diploma in Leadership and Quality in Healthcare from the Royal College of Physicians in Ireland, an Advanced Diploma in Executive Coaching and a graduate award in Executive Healthcare Leadership from the Health Service Leadership Academy.
Professionally, Louise has worked closely with the Irish Association of Speech and Language Therapists (IASLT) having previously been a member of the Validation Committee and is currently Chair of the Education Board.
Marian Vaughan
 Marian was elected to the Board last year in Category B, Children’s Nursing and currently works as the Clinical Placement Coordinator (CPC) in CHI at Crumlin. She is registered in the General and Children’s Divisions of NMBI Register of Nurses and Midwives. Marian became a RGN in 1988 and a RCN five years later, completing a Diploma in Pharmacology at RCSI in 1991. She obtained her Bachelor’s Degree in Nursing Studies at DCU in 2010.
Marian was elected to the Board last year in Category B, Children’s Nursing and currently works as the Clinical Placement Coordinator (CPC) in CHI at Crumlin. She is registered in the General and Children’s Divisions of NMBI Register of Nurses and Midwives. Marian became a RGN in 1988 and a RCN five years later, completing a Diploma in Pharmacology at RCSI in 1991. She obtained her Bachelor’s Degree in Nursing Studies at DCU in 2010.
Marian has 32 years’ nursing experience, with 27 years in children’s nursing with experience in Infant Cardiology in both New Zealand and in Crumlin. She has extensive Neonatal Intensive Care Unit experience and has been a Research nurse in two studies in a UCD academic-clinical partnership. Her experience includes a decade as a Clinical Nurse Facilitator at CHI and 15 years membership of Nurse Practice and Nurse Education Committees.
Marian has also been project leader in an initiative which led to the development of a Standardised Cross-Hospital Student Evaluation Programme, as part of the CHI Quality Improvement and Patient Safety Programme.
Siobhan McArdle
 Siobhán is currently an Assistant National Director in the HSE with responsibility for Covid-19 Operations. She holds a senior leadership role in the operational design and delivery of new Covid-19 services at local and national level as part of the HSE's pandemic response. She is also a member of the Working Group for the High Level Task Force on Covid-19 vaccination.
Siobhán is currently an Assistant National Director in the HSE with responsibility for Covid-19 Operations. She holds a senior leadership role in the operational design and delivery of new Covid-19 services at local and national level as part of the HSE's pandemic response. She is also a member of the Working Group for the High Level Task Force on Covid-19 vaccination.
A qualified Speech and Language Therapist, she presents with almost 30 years’ experience of working in a range of local, regional and national healthcare services in clinical, management and leadership roles. As a senior healthcare manager, she has an established track record of working collaboratively and strategically with others, making links across the wider healthcare system, governmental departments and external agencies, to facilitate and enable improvements in service delivery.
In addition to her clinical training, Siobhán holds an M.Phil and postgraduate qualifications in corporate governance and leadership.