|
NMBI Hosts Inaugural Irish Interprofessional Healthcare Regulatory Symposium
On 21 November, NMBI hosted the inaugural Irish Interprofessional Healthcare Regulatory Symposium. The event brought together Board members, CEOs and Directors from the five healthcare regulators – NMBI, CORU, the Dental Council, the Medical Council, the Pharmaceutical Society of Ireland.

On 21 November, NMBI hosted the inaugural Irish Interprofessional Healthcare Regulatory Symposium. The event brought together Board members, CEOs and Directors from the five healthcare regulators – NMBI, CORU, the Dental Council, the Medical Council, the Pharmaceutical Society of Ireland.
We were delighted to be joined by Rachel Kenna, the Chief Nursing Officer and colleagues at the Department of Health.
The symposium is a key professional event bringing together representatives from Ireland’s healthcare regulators to collaborate and reflect on the system-wide challenges and opportunities.

Our President, Dr Louise Kavanagh McBride opened the event saying the “The symposium is designed for us, as Irish regulators, to reflect on the pressures, risks and challenges currently facing the regulatory sector, as well as allowing us to focus on the strengths and the opportunities available.”
Lisa Manselli, Executive Consultant in Regulation, hosted a Fireside Chat with the CEOs who highlighted the key areas impacting the regulatory landscape in Ireland.
Two breakout sessions took place with delegates discussing the challenges and opportunities for Irish healthcare regulators.
The event was an important occasion to strengthen relationships across regulators and identity areas of collaboration.
We would like to thank everyone who participated for their engagement and for sharing their views.
2026 Annual Registration Renewal Now Open
The 2026 annual registration renewal window is open. Registrants can renew online up to 31 January 2026.
All nurses or midwives practising in Ireland are required by law to have their name on the Register of Nurses and Midwives which is maintained by NMBI and each year it is necessary to pay the annual renewal to maintain registration.
The 2026 annual registration renewal window is open. Registrants can renew online up to 31 January 2026.
All nurses or midwives practising in Ireland are required by law to have their name on the Register of Nurses and Midwives which is maintained by NMBI and each year it is necessary to pay the annual renewal to maintain registration.
Student nurses and midwives, as well as those who have registered for the first time, on or after 1 September 2025, are not required to renew until the 2027 annual renewal cycle.
Notices containing details on how to renew have been issued by email to all registrants. If you have not received your notice, please check your spam, junk or other email folders. If your email is not in these folders, you can contact our customer care centre at 0818 200 116 (+353 818 200 116 from outside Ireland) or email regservices@nmbi.ie and we will send you the details. When contacting us, please provide your name, Personal Identification Number (PIN) and date of birth to ensure we can deal with your query efficiently.
Completing the annual renewal process
The annual renewal process must be completed through our online portal, MyNMBI. The portal has recently been upgraded to ensure the renewal process is as user-friendly as possible. While the portal may look different, the process is the same and will only take a few minutes to complete. Your username has not changed; however, you will need to change your password to access your account. Payments cannot be made by phone.
To assist registrants through the annual renewal process, we have created a step-by-step video as well as helpful guides. We advise that registrants view these before renewing. The guides can be found on our website.
Please note that due to the large number of registrants who need to renew with NMBI, there may be times when the MyNMBI portal is slower processing details and payment, due to high level of usage at any one time. If you experience this issue, we suggest that you log out and come back to the portal later. Peak usage tends to be in the evenings from 6pm to 7pm.
While the annual renewal window is open until 31 January 2026, we encourage registrants to login and renew online as soon as possible to avoid any delays in processing during peak times.
When completing your annual registration renewal, you must ensure that all your details are correct and up to date. This is a legal requirement under Section 53 of the Nurses and Midwives Act 2011, as amended.
We are required to collect your contact information (address, email address and phone number). We also collect your employment details including job title, workplace and the divisions of the Register you are practising in. NMBI has a legal requirement to gather this information to ensure public safety and protect our registrants.
You will also be required to read and declare that the information you provided is accurate. This is an important part of your registration.
Support
For those who require assistance to complete the renewal process, please call 0818 200 116 (+353 818 200 116 from outside Ireland), open Monday to Friday, 9am - 5:30pm or email our Registration Department at regservices@nmbi.ie. When contacting us, please provide your name, Personal Identification Number (PIN) and date of birth to ensure we can deal with your query efficiently.
How do you voluntarily remove if you do not want to renew?
You can voluntarily remove your name from the Register of Nurses and Midwives on MyNMBI. This service is free of charge and will be available during the renewal period. You must select every division you awish to be removed from. Should you choose this option you can restore your name to the Register at any time by selecting the Restoration option on the MyNMBI portal.
What happens if you do not renew your registration?
All nurses and midwives who practise in Ireland must, by law, be listed on the Register of Nurses and Midwives. Practice includes clinical practice, nursing or midwifery management, education and research.
If you do not renew your registration for 2026, or voluntarily remove yourself, your name will be removed from the Register for non-payment of the renewal fee (Section77 (1) of the Nurses and Midwives Act 2011, as amended). Please note that notifications of removals are sent to employers, the Minister for Health and the Health Service Executive (under Section 82 of the Act).
Restoration following removal for non-payment of the annual registration renewal
If your name is removed from the Register for non-payment of your annual renewal fee (Section77 (1) of the Nurses and Midwives Act 2011, as amended) and you subsequently wish to restore your name to the Register, a restoration fee of €250 in addition to your annual renewal fee will apply. You will also need to comply with the restoration requirements at the time of application.
What your annual registration renewal is used for
Your annual registration renewal goes towards our work to support nurses and midwives to provide the highest standards of professional practice. Through our registration, education and guidance, and fitness to practise functions we enhance the safety of people using services. Further information about the work we do can be found on our website.
|
|
New NMBI State of the Register 2025 Report Published
We have published our State of the Register 2025 report which shows that as of 1 June 2025, there were 92,385 nurses and midwives on the NMBI Register, 86,948 who state that they are currently practising and 79,194 who are patient-facing.

We have published our State of the Register 2025 report which shows that as of 1 June 2025, there were 92,385 nurses and midwives on the NMBI Register, 86,948 who state that they are currently practising and 79,194 who are patient-facing.
The publication, now in its fourth edition, provides an overview of the composition and trends within Ireland’s nursing and midwifery professions. In 2022, the first published State of the Register showed that 81,431 nurses and midwives were registered. In 2025, there are 92,385 registrants recorded, showing an overall increase of 13.45% over the four years.
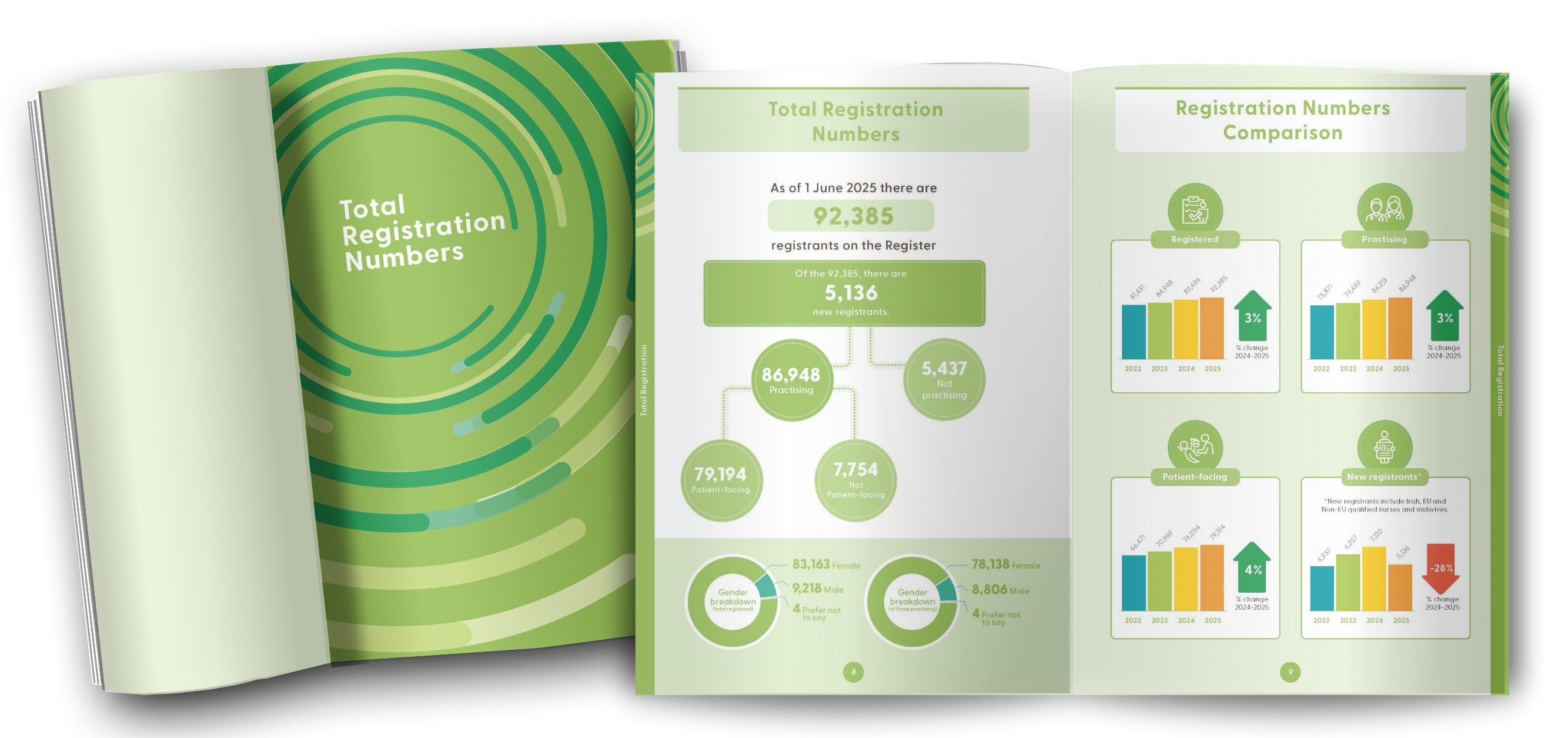
The data contained in the report provides robust evidence to inform workforce planning, policy formulation and strategic decision-making across the Irish health sector.
Minister for Health, Jennifer Carroll MacNeill commented on the report, stating, “The number of Irish-educated graduate nurses and midwives coming onto the NMBI Register is increasing year on year. In addition, Irish educated and registered nurses and midwives are opting to stay and practise in Ireland. This is positive news and is important for workforce planning and long-term stability in our health services.”
Chief Nursing Officer, Rachel Kenna, added, “This latest State of the Register Report provides clear, reliable data and important insights that can inform policy development and decision-making.
The information is central in helping to shape better policies to support and empower nurses and midwives and advance their practice, while ensuring the highest standards of public safety.”
NMBI President, Dr Louise Kavanagh McBride, said: “This report is a valuable resource for policymakers and workforce planners, supporting evidence-based decisions that enhance healthcare delivery across Ireland. It acts as an important tool for our colleagues across the health sector, as we collectively strive to strengthen healthcare delivery and ensure public confidence in nursing and midwifery.
As a regulator, we continue to advance the standards of nursing and midwifery in Ireland for the benefit of patients, service users, communities and society.”
NMBI Chief Executive Officer, Carolyn Donohoe, remarked, “The comprehensive data, provided in the NMBI State of the Register, supports our collective efforts to ensure the Irish healthcare system is equipped to meet future needs. It is heartening to note that there are now 92,385 nurses and midwives on the NMBI Register, which is a 3% increase on the previous year, and the highest number recorded to date.”
The State of the Register 2025 report provides an in-depth look into the registration data for the nursing and midwifery professions in Ireland. It is available for download on the NMBI website.
The data is based on the information collected by NMBI as part of the annual renewal process. Data is compared annually in June each year and covers the 12-month period from 1 June 2024 to 31 May 2025.
Overview of the data
As of 1 June 2025, there were 92,385 nurses and midwives on the NMBI Register, which represents a 3% increase on the previous year. It is the largest number of registered nurses and midwives recorded to date. The number of practising and patient facing registrants has also increased. 86,948 nurses and midwives state that they are currently practising (a 3% increase) and 79,194 state they are patient-facing (a 4% increase).
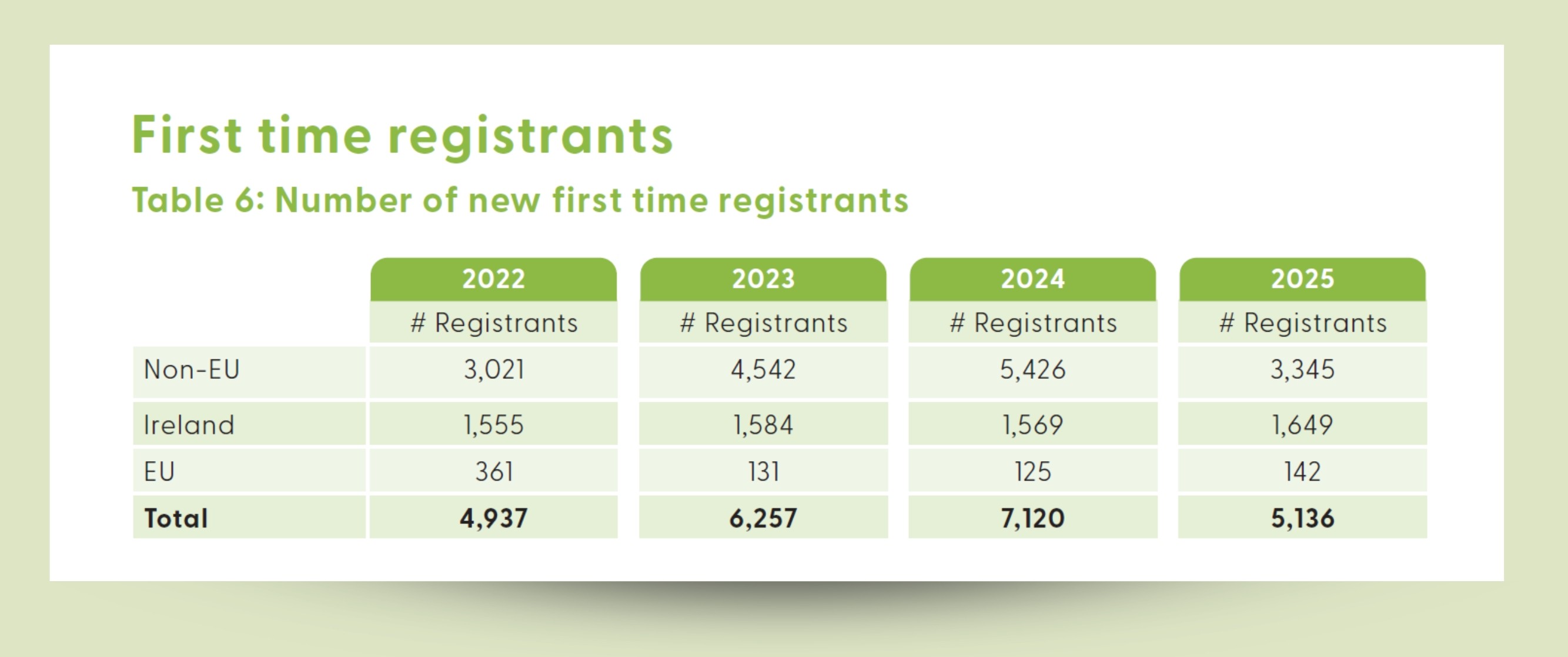
5,136 new registrants joined the NMBI Register in the period, including Irish and internationally educated nurses and midwives. While there has been a decrease in the number of new registrants who were educated abroad, there has been a consistent increase in the number of Irish graduates joining the Register. In 2025, 1,649 new Irish-educated nurses and midwives were added to the NMBI Register, up 5% (1,569) on 2024 figures.
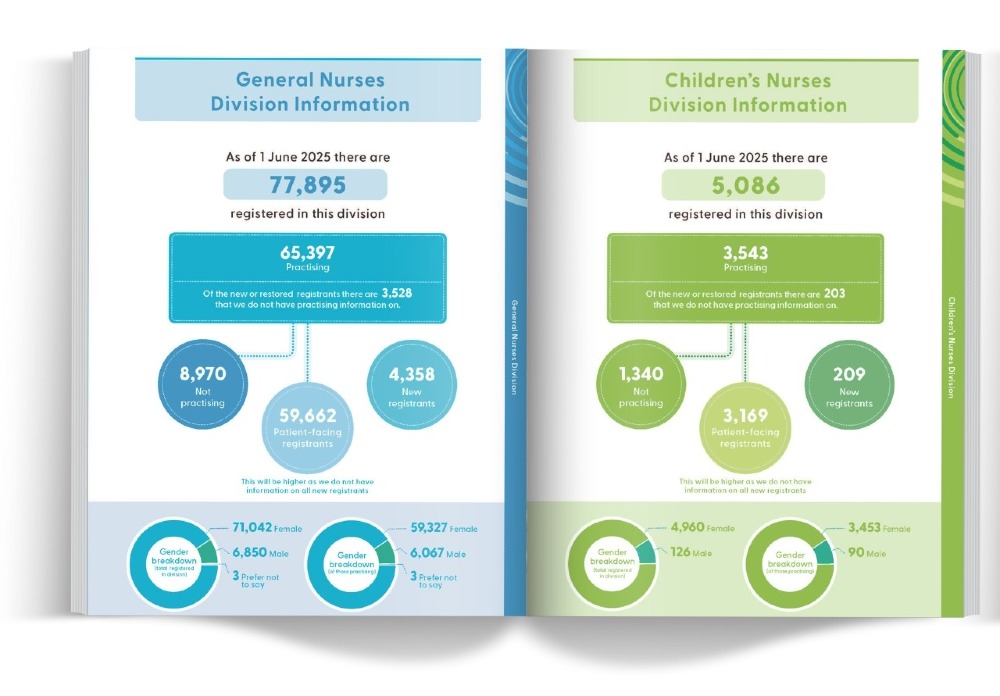
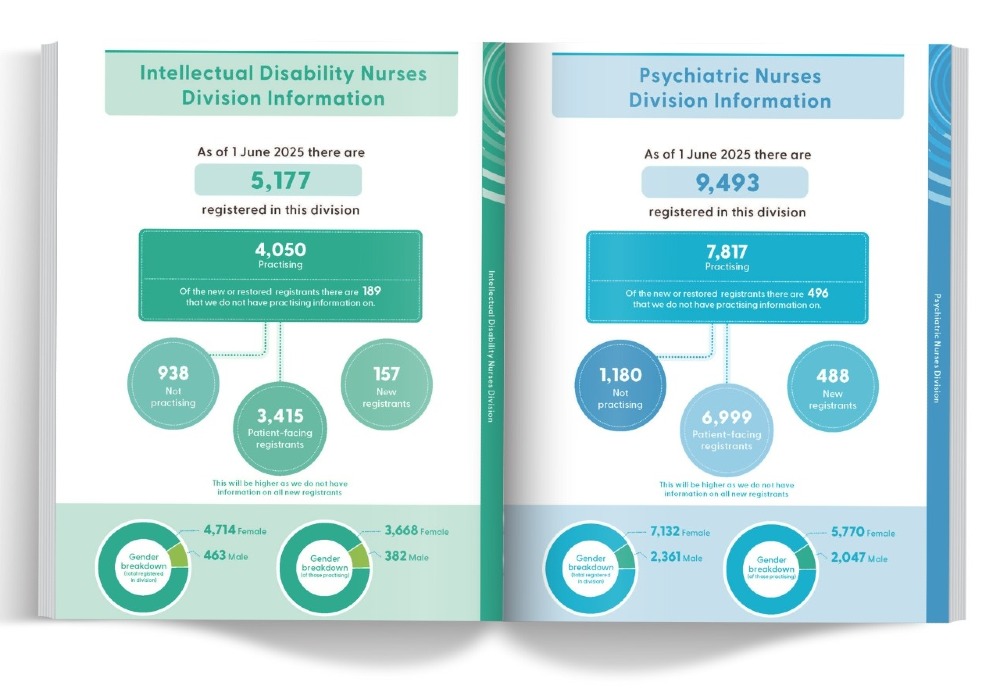
On a divisional level, there were increases in the number of registered General Nurses (3%); Psychiatric Nurses (2%) and Children’s Nurses (1%) while the number of Intellectual Disability Nurses remained the same (0.4%).
The number of registered Midwives decreased (3%), while the division saw an increase in the numbers practising (2%) and patient-facing (3%).
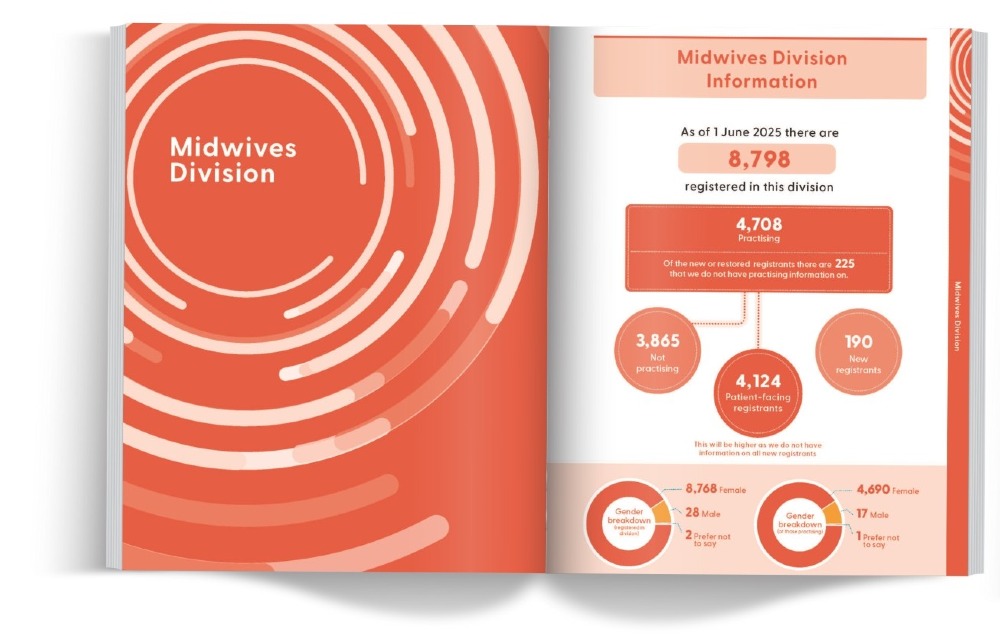
There has been sustained growth in the post-primary divisions of the Register, reflecting continuing professional development and diversification within the professions. There was a 24% increase in Advanced Nurse Practitioners (total of 1,204 on the register) and an 8% increase in Advanced Midwife Practitioners (total of 40 on the register). Nurse Prescribers increased by 15% (total of 2,963 on the Register, and Midwife Prescribers increased by 26% (total of 132 on the Register). The number of registered Public Health Nurses increased marginally by 1% (total of 2,780 on the Register).


Advanced practice is a career pathway for registered nurses and midwives, committed to continuing professional development and clinical supervision, to practise safe and effective person-centric care at a higher level of capability as independent, autonomous, and expert practitioners.
Since June 2023, there has been a steady decrease in the number of registered nurses and midwives requesting a Certificate of Current Professional Status (CCPS) from NMBI to work abroad. A CCPS is required by regulators in other jurisdictions to confirm an individual’s good standing before they can practise abroad. This downward trend in CCPS applications suggests that fewer nurses and midwives are choosing to seek registration to work in another jurisdiction.
Focus on Fitness to Practise in New Episode of NMBI Voice
The latest episode of our podcast, NMBI Voice is now available and this month, fitness to practise is our focus as Kathyann Barrett speaks to Marie-Therese Hackett, our Inquiries Legal Adviser about how fitness to practise protects public safety.
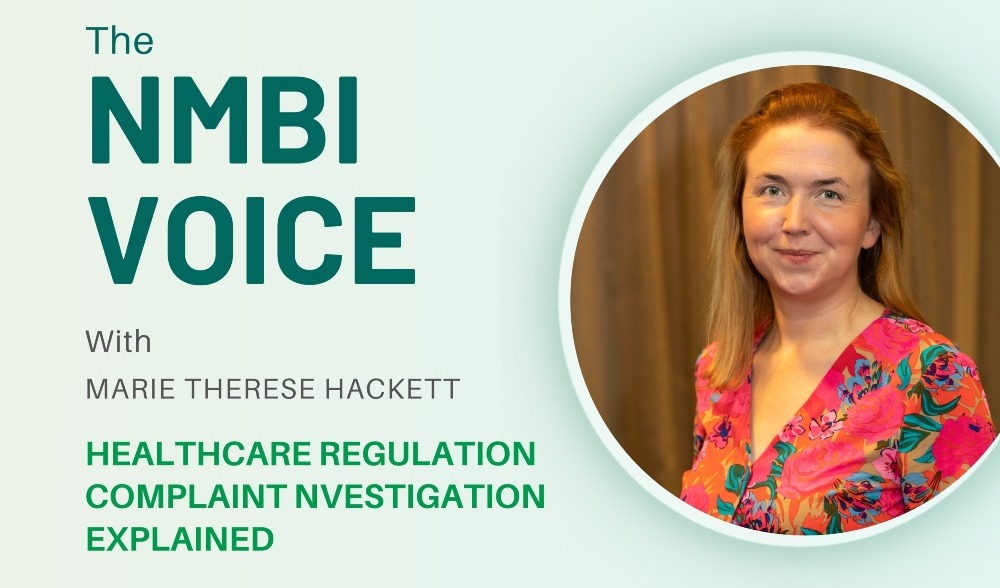
The latest episode of our podcast, NMBI Voice is now available and this month, fitness to practise is our focus as we hear from Marie-Therese Hackett, our Inquiries Legal Adviser.
Fitness to practise sounds intimidating and for nurses and midwives facing complaints, it can feel like the hardest side of regulation.
Marie-Therese speaks to Kathyann Barrett about how fitness to practise protects public safety and how the three-stage legal framework for complaints works.
A key area of focus for Marie-Therese is NMBI’s Compassion Project. In this episode, she explains how the Compassion Project transformed witness care through a dedicated liaison officer and 24/7 emotional support line. She also discusses why witnesses experience re-traumatisation without trauma-informed practices and how reducing ‘witness work’ through practical measures supports participants.
Marie-Therese has 20 years’ experience in the legal profession working across criminal law, civil litigation, and healthcare regulation. Her professional background provides a strong foundation for ensuring regulatory processes are fair, transparent, and proportionate. Having worked closely with vulnerable participants in a range of legal processes and regulatory systems, she is deeply aware of the impact such processes can have on the individual.
These experiences have made her passionate about promoting compassionate practice and reducing harm wherever possible. Marie-Therese’s personal experience of neonatal intensive care units has given her a profound respect for healthcare professionals and a deep appreciation of the trust that patients and their families place in the healthcare system. These personal experiences strengthen her commitment to fairness, empathy, and continuous improvements in healthcare regulation.
Listen now on Apple, Spotify or wherever you get your podcasts.
_______________

NMBI Voice launched in September and each episode covers different areas of our work, as well as the key changes and challenges facing our professions today. We aim to break down complex topics and offer practical guidance you can use.
You can listen back to previous episodes through the links below.
Episode 1: From Principles to Practice: The NMBI Code
Episode 2: Keeping Practice Safe: Inside NMBI’s Professional Competence Scheme
Episode 3: Realities of Registration
New episodes air on the first Monday of every month. Make sure to follow NMBI Voice to stay up to date as new episodes air.
Dr Joanne O’Brien Kelly Becomes First Nurse Elected to the EFIC Board
Dr Joanne O’Brien Kelly, an ANP in Pain Management has become the first nurse to be elected to the Board of the European Pain Federation (EFIC).

Pictured (L to R): Professor Patrice Forget; Dr Joanne O’Brien Kelly and Liisa Jutila
Dr Joanne O’Brien Kelly, an Advanced Nurse Practitioner in Pain Management from Beaumont Hospital, has become the first nurse to be elected to the Board of the European Pain Federation (EFIC).
Dr O’Brien Kelly’s leadership exemplifies how the NMBI Code of Professional Conduct and Ethics (2025) guides nursing at advanced practice levels.
The Code applies to all nurses and midwives, at every grade and in every setting. It sets out the professional conduct expected of our registrants and their obligation to practise in line with the six core principles — Respect, Accountability, Competence, Trust, Collaboration and Leadership. In her role as an Advanced Nurse Practitioner, Joanne demonstrates how these principles translate into action: leading by example in delivering best practice, keeping patients’ needs at the centre, and showing how nurses can lead the profession forward through advocacy, innovation and influence at policy level.
On 16 October, the European Pain Federation (EFIC) endorsed the Societal Impact of Pain (SIP) platform a high-level policy event ‘From Burden to Prevention: Reframing Chronic Pain in EU Health Policy’ at the European Parliament in Brussels.
Moderating the discussion was Dr O’Brien Kelly and Vice Chair of the Advocacy Committee. She was pivotal in bridging the lived-experience and clinical practice perspectives, fostering inclusive dialogue on how prevention can be operationalised across health systems and emphasising the role of nursing and advanced practice in that agenda.
The European Pain Federation EFIC is an organisation representing over 20,000 health care professionals from the field of pain management and pain science from 39 countries.
The event was attended by Dan-Stefan Motreanu, MEP, Sirpa Pietikäinen MEP, Vytenis Povilas Andriukaitis, MEP and Tomislav Sokol, MEP. Speakers included Professor Patrice Forget as EFIC/SIP Chair; Liisa Jutila, from Pain Alliance Europe (PAE) a patient organisation; Amy Jo Collins from the World Health Organisation; Anna van Renen from the International Longevity Centre UK and Dr Mary O’Keeffe from University College Dublin.
New School of Nursing at Maynooth University Launched Following NMBI Approval
Congratulations to Maynooth University (MU) who officially launched a new School of Nursing last month following NMBI approval.

Pictured (L to R): Minister for Further and Higher Education James Lawless, TD; Kate Killeen White, Regional Executive Officer, HSE Dublin and Midlands Region; Founding Head of the School of Nursing Prof Fintan Sheerin, Rachel Kenna, Chief Nursing Officer at the Department of Health; Carolyn Donohoe, NMBI CEO; Michael J Dowling, CEO Emeritus of Northwell Health and MU President Prof Eeva Leinonen
Congratulations to Maynooth University (MU) who officially launched a new School of Nursing last month following NMBI approval.
At the launch, our CEO, Carolyn Donohoe along with Rachel Kenna, Chief Nursing Officer at the Department of Health and Kate Killeen White, Regional Executive Officer of the HSE Dublin and Midlands Region took part in a panel discussion, chaired by Professor Fintan Sheerin, Founding Head of the MU School of Nursing.
The new School was established by Professor Sheerin and his colleagues Dr Adeline Cooney, Dr Myles Hackett and Emma Guyatt.
The launch at Maynooth University was officially opened by Minister for Further and Higher Education, Research, Innovation and Science, James Lawless, TD.
|
|
Spotlight Series On: Spark Innovation Programme - My Journey from Midwife to Innovator
By Una Rogers
When I graduated with a BSc in Midwifery from Dundalk Institute of Technology in 2014, Ireland was still in the grip of a financial crisis. The HSE recruitment embargo meant that, for direct-entry midwives, employment opportunities were scarce. In fact, on graduation day we were handed leaflets for the NHS, an unmistakable sign of the challenges ahead.

When I graduated with a BSc in Midwifery from Dundalk Institute of Technology in 2014, Ireland was still in the grip of a financial crisis. The HSE recruitment embargo meant that, for direct-entry midwives, employment opportunities were scarce. In fact, on graduation day we were handed leaflets for the NHS, an unmistakable sign of the challenges ahead.
This early experience shaped my understanding of what it meant to qualify as a direct-entry midwife during that time. After seven years working as a labour ward midwife in the Coombe and Galway University Hospital, I took a leap into management and became a CMM2 in the labour ward at Portiuncula University Hospital in 2021. It was there that I truly found my voice.
Confident in my practice and knowledge, I began to question long-standing processes: Why do we do it this way? Can we do better? Should we be better? When can we change? Supported by an exceptional ADOM and DOM and guided by my MSc in Midwifery Leadership from Trinity College Dublin, I began using audit and quality improvement methodologies to address issues such as the induction-of-labour process through an IOL working group and enhanced staff education.
This work sparked a deeper passion for innovation. I found myself constantly examining systems and imagining what could be improved. In the post-Covid landscape, I felt that midwives were ready to reimagine and redesign care. We had weathered extraordinary challenges together and proven our ability to adapt rapidly and safely.
Identifying a significant gap in digital health, I turned my attention to women’s health technologies. When I transitioned into the role of Maternity OPD Manager, I quickly encountered issues with translation services. Face-to-face interpreters were costly, difficult to schedule, and introduced another person into highly sensitive clinical conversations.

With the support of hospital general management and Spark Innovation Seed funding, I piloted a proof-of-concept project using a translation app within the Maternity OPD. The results were immediate and impactful. Energised by its success, I championed the project across the HSE, eventually connecting the developers with the HSE’s eHealth division, an introduction that has now led to a nation-scale pilot across three clinical sites.
A second successful innovation project, supported by another Spark Seed award in Galway University Hospital, gave me the confidence to take my next big step: applying for the Spark Innovation Fellowship. With experience in frontline innovation and a deep commitment to improving healthcare, particularly for women, I was honoured to be selected. I began my National Nursing and Midwifery Innovation Fellowship with the Spark Innovation Programme in July of this year.
The past four months have been transformative. I have had the privilege of supporting nurses and midwives across Ireland as they take their first steps into innovation. I have mentored colleagues, encouraged them to pursue their ideas, and contributed to national discussions on digital transformation within nursing and midwifery.
 For someone who once almost followed that NHS leaflet across the Irish Sea, I now feel that my opportunities are limitless. My journey as a direct-entry midwife has grown into a career defined by curiosity, courage, and a belief in better. For someone who once almost followed that NHS leaflet across the Irish Sea, I now feel that my opportunities are limitless. My journey as a direct-entry midwife has grown into a career defined by curiosity, courage, and a belief in better.
I truly believe the world is mine for the taking, and I cannot wait to continue representing midwifery every step of the way.
The Spark Innovation Programme is a frontline, staff-led initiative that seeks to support, promote and recognise innovation amongst healthcare staff. Spark is about shared learning and creating an empowering work environment for healthcare professionals to bring their creativity, imagination, problem solving skills, love of design, and passion for the wellbeing of patients/women.
Meet Our Midwifery Student Ambassador: Katelyn Cahill
In this month’s issue, we speak with Katelyn, a 3rd Year Midwifery student at University College Dublin. Her story highlights her profound love for midwifery and how, her placement experiences have affirmed her belief that supporting women and families through childbirth is not just a profession, but a privilege. Her journey highlights the joy, meaning, and fulfilment she has found in a role that allows her to make a real difference in people’s lives.

My name is Katelyn and I am in my 3rd Year of the BSc Midwifery course at University College Dublin.
I always loved hospitals and knew that I wanted some sort of medical career but during my leaving certificate I was torn between a few different courses. Midwifery was my top choice, but it was the highest points. I honestly didn't think that I would get in. Well, here I am!
The first few weeks of my course were spent feeling like an imposter among the other students. I worried that midwifery wouldn’t be for me. So many of the others had worked hard to get in and had wanted to be a midwife for years.
 My first placement was three months into the course and that was when everything changed. I have genuinely never felt such a love or passion for something before. My family says that I light up when speaking about anything to do with midwifery and women's health. I have always had strong opinions about women's rights and feminism so being in a job that allows me to advocate and empower women daily fulfils me more than I had imagined. I have never felt more like I belong than when I am caring for women and doing everything in my power to make them feel seen, safe and cared for. My first placement was three months into the course and that was when everything changed. I have genuinely never felt such a love or passion for something before. My family says that I light up when speaking about anything to do with midwifery and women's health. I have always had strong opinions about women's rights and feminism so being in a job that allows me to advocate and empower women daily fulfils me more than I had imagined. I have never felt more like I belong than when I am caring for women and doing everything in my power to make them feel seen, safe and cared for.
For me, being a midwife is about so much more than medically caring for women. During my placements in first year, I had limited capabilities, and I honestly think it taught me some of my most valuable lessons. While the midwives were busy caring for the women’s medical needs, my limited skills allowed me the opportunity to emotionally support the women through their journey. I was able to hold her hand as she pushed, be a shoulder to cry on if things weren’t going her way and talk her through everything that was happening around her.
 There is nothing that could compare to the feeling of knowing that you made even the slightest bit of a difference to a woman's journey. I have held this value with me since and I intend to use it in all the years that I practice as a midwife. There is nothing that could compare to the feeling of knowing that you made even the slightest bit of a difference to a woman's journey. I have held this value with me since and I intend to use it in all the years that I practice as a midwife.
I am now three years into my journey to become a midwife and my love and passion for it has not dampened one bit. I am truly privileged to be part of a team that supports families around their journey of bringing life into the world. In no way am I exaggerating when I say it is the best job in the world.
|
|
Our Interim Director of FTP Speaks at Healthcare and Regulatory Conference
Last month, our Interim Director of Fitness to Practise, Yvanne Kennedy took part in a panel discussion about the complaints and investigations process at a Healthcare and Regulatory Conference.

Last month, our Interim Director of Fitness to Practise, Yvanne Kennedy took part in a panel discussion about the complaints and investigations process at a Healthcare and Regulatory Conference.
The panel included Dr Suzanne Crowe, President of the Medical Council as well as senior lawyers. The discussion covered topics about compassion in fitness to practise, the use of social media by professionals and handling complaints at the earliest stage of the fitness to practise process.
The Healthcare and Regulatory Conference, a cross-border event with speakers from Ireland and Northern Ireland, was hosted by law firm Carson McDowell.
The theme of the conference was Legal Systems and Health Services: Cross-Border Learning in Healthcare Law and was attended by more than 100 legal and regulatory professionals.
Advanced Practice Conference Celebrates Collaboration in Maternity Care
Our Director of Professional Standards – Midwifery, Dr Karn Cliffe recently attended the Advanced Practice Conference along with AMPs and ANPs from maternity and acute settings.

Our Director of Professional Standards – Midwifery, Dr Karn Cliffe recently attended the Advanced Practice Conference along with Advance Midwife Practitioners and Advance Nurse Practitioners from maternity and acute settings.
The conference, held at the Rotunda Hospital, highlighted how collaboration is improving care for pregnant women and their babies.
Throughout the day, experts shared real-life examples of this successful collaboration. Presenters included Advanced Practitioners from the Rotunda, the Coombe, the Mater Misericordiae and Beaumont Hospitals, as well as staff from Trinity College Dublin’s School of Midwifery and a Consultant Obstetrician from the Rotunda Hospital.
Karn discussed the topics as part of a round table discussion with Fiona Hanrahan, Professor Deirdre Daly, Rhona Savage and Bernie Gregg.
The collaborative, woman-centred approach of midwives, nurses, obstetricians, neonatologists and specialty services focuses on the safest possible outcomes for mothers, babies, and families.
Compassion in Fitness to Practise Process Highlighted at HSE ADONM Conference
Our Interim Director of Fitness to Practise, Yvanne Kennedy recently spoke at the HSE Midwest Acute Hospital ADONM Conference.

Our Interim Director of Fitness to Practise, Yvanne Kennedy recently spoke at the HSE Midwest Acute Hospital, Assistant Director of Nursing and Midwifery (ADONM) Conference.
In her presentation, Yvanne highlighted the important work NMBI is doing to ensure we are a more supportive and compassionate regulator. She also outlined how the Code and maintenance of professional competence guide registrants in their practice. Through the Compassion Project, we are actively taking steps to improve the fitness to practise process, and we continue to develop supports for registrants and for those assisting with the process.
The conference, held in University Hospital Limerick, was an opportunity to share knowledge about local and national projects affecting nursing and midwifery in the Midwest. Attendees also heard from one of the keynote speakers, Rachel Kenna, Chief Nursing Officer at the Department of Health.
|
|
|