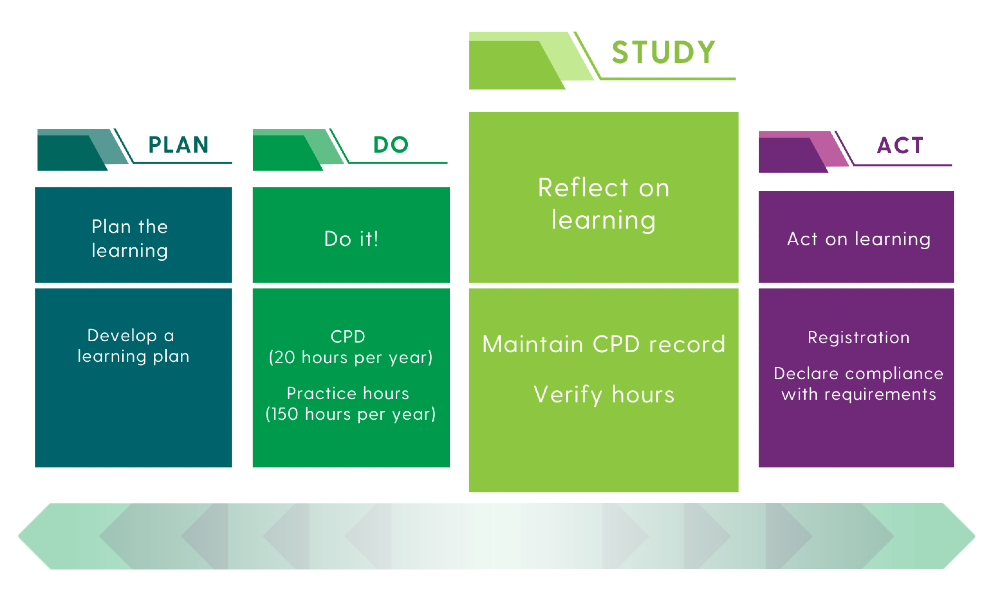
The Professional Competence Scheme (PCS) is based on the PDSA Quality Improvement Tool, (Plan, Do Study, Act). The Study phase of the PCS focuses on Reflection.
Reflective practice encourages practitioners to think deeply about experiences and find new meaning in their current ideas or ways of doing things. It can reveal gaps in knowledge and boost critical thinking and independent learning.
For practitioners, reflective practice helps to apply new knowledge and support change. Better knowledge and assessment skills lead to improved care planning and better outcomes for individuals with healthcare needs. Ongoing learning from reflective practice helps practitioners grow as professionals within a team, promoting critical thinking, clear communication, and teamwork – all vital for delivering high-quality care (Patel & Metersky 2022).

This evidence is reflected in our feature article below by Clinical Nurse Specialist, Siobhan McMahon, a PCS pilot participant at Our Lady of Lourdes Hospital, Drogheda. Siobhan describes how engaging in reflection has not only supported the maintenance and development of her professional competence but has also enhanced the quality and safety of the care she provides.
For more information on Reflection, visit our new webpage.
Enhancing Professional Practice through the NMBI Professional Competence Scheme Pilot

Participating in the Nursing and Midwifery Board of Ireland (NMBI) Nursing Professional Competence Scheme Pilot is an enriching experience that has significantly influenced my role as a Clinical Nurse Manager 2 (CNM 2) specialising in Inflammatory Bowel Disease (IBD).
Recently, I had the opportunity to attend a webinar hosted by the Irish Cancer Network, which explored the impact of alcohol, smoking, and nutrition on cancer risk, particularly for patients with conditions like IBD who face an increased likelihood of developing certain cancers. The key takeaway reinforced the critical importance of holistic patient care, emphasising our role not only in managing the IBD itself but also in educating patients about broader health risks and lifestyle factors.
Central to my professional responsibilities is the principle of accountability, as outlined in the nursing Code of Professional Conduct and Ethics (2025). This includes maintaining and developing specific competencies related to planning, prioritising, and delivering patient-centered care through both clinical interventions and patient education.
The structured framework of the professional competence scheme encourages me to engage in critical self-reflection, assessing my skills, knowledge, and areas for development. This process has deepened my awareness of the specialist role I hold in caring for patients with IBD and motivates me to continually enhance my clinical abilities.
Through fulfilling the scheme’s requirements, I am identifying targeted competencies to develop, which has boosted my confidence and effectiveness in delivering safe, evidence-based care. Overall, the pilot is reinforcing my commitment to lifelong learning and continuous professional growth, ensuring the highest standards of care for my patients.