
The Critical Care ANP Team, St James’s Hospital, Dublin
As the largest cohort of healthcare employees, nurses play a pivotal role in global healthcare reform. In March 2020, the Critical Care Advanced Nurse Practitioner (CCANP) service was developed by a team of Advanced Nurse Practitioners (ANP) at St James’s Hospital (SJH), Dublin. The service was established in response to the Irish Government’s Critical Care Strategic Plan. The aim of this plan is to increase critical care bed capacity, to target the under provision of intensive care unit beds and meet the national key performance indicators related to admission targets for critically ill patients.
The CCANP team in St James’s Hospital is just one of approximately 43 specialities and subspeciality ANP services available at the hospital. Comprised of eight experienced intensive care nurses, the CCANP team strive to make a meaningful difference to the deteriorating critically ill patient throughout the hospital.
The CCANP team, are purpose driven and results focused, with a commitment to advancing nursing, strengthening staff capability, promoting nurse research and leadership, and pursuing excellence in patient outcomes.
Our ANP service is divided into a four-pillar approach underpinned by research and audit. The pillars consist of patient care in pre-ICU, in ICU and post-ICU, with education provision allowing for the empowerment of both patients and hospital staff. This approach ensures CCANPs involvement in patient care from the moment of deterioration to discharge from ICU and includes attendance at the ICU recovery clinic from home.
The fundamental premise is that to achieve optimal patient outcomes and nurse satisfaction, nurse competencies must be driven by patient and service need in alignment with the HSE (2014) vision of ICU without walls, ensuring the ‘right patient, is with the right people, in the right place, at the right time’.
Admitting patients to the ICU as quickly as possible is crucial because delayed admission to critical care is strongly associated with increased morbidity, higher mortality rates and longer hospital stays.
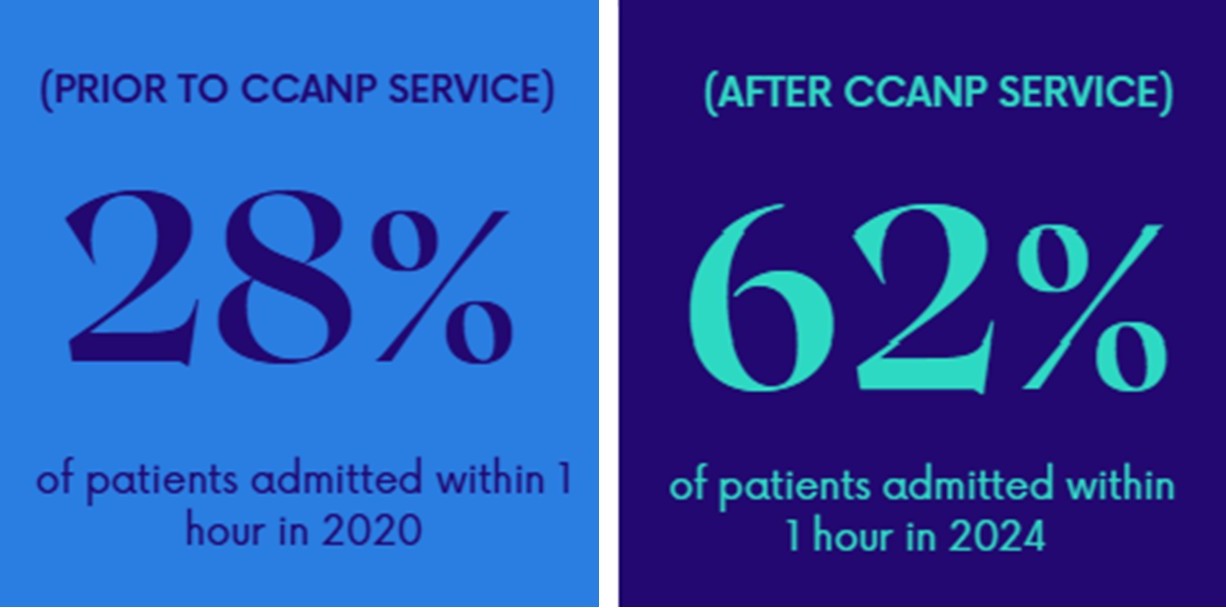
The CCANP team’s admission Key Performance Indicator targets for critically ill patients are benchmarked against the National Office of Clinical Audit data, 2023: 50% of patients should be admitted within one hour of the decision to admit and 80% of patients should be admitted within four hours of the decision to admit.
In partnership with nursing, medical and multidisciplinary colleagues, and with the provision of the emergency bed, the CCANP team have superseded these admission targets. In 2024, the CCANP service facilitated 50% of unplanned admissions. 62% were admitted within one hour and 99% were admitted within four hours.
Once a decision has been made to admit the patient, a member of the CCANP team is immediately available to manage the deteriorating patient on the ward and facilitate enroute procedures. When enroute procedures or investigations are taken into consideration, 85% of patients were admitted within one hour. This is important to note, as we are patient focused, not KPI driven. It is more important for this cohort of patients to receive efficient prognostication than to be expediated to the ICU.
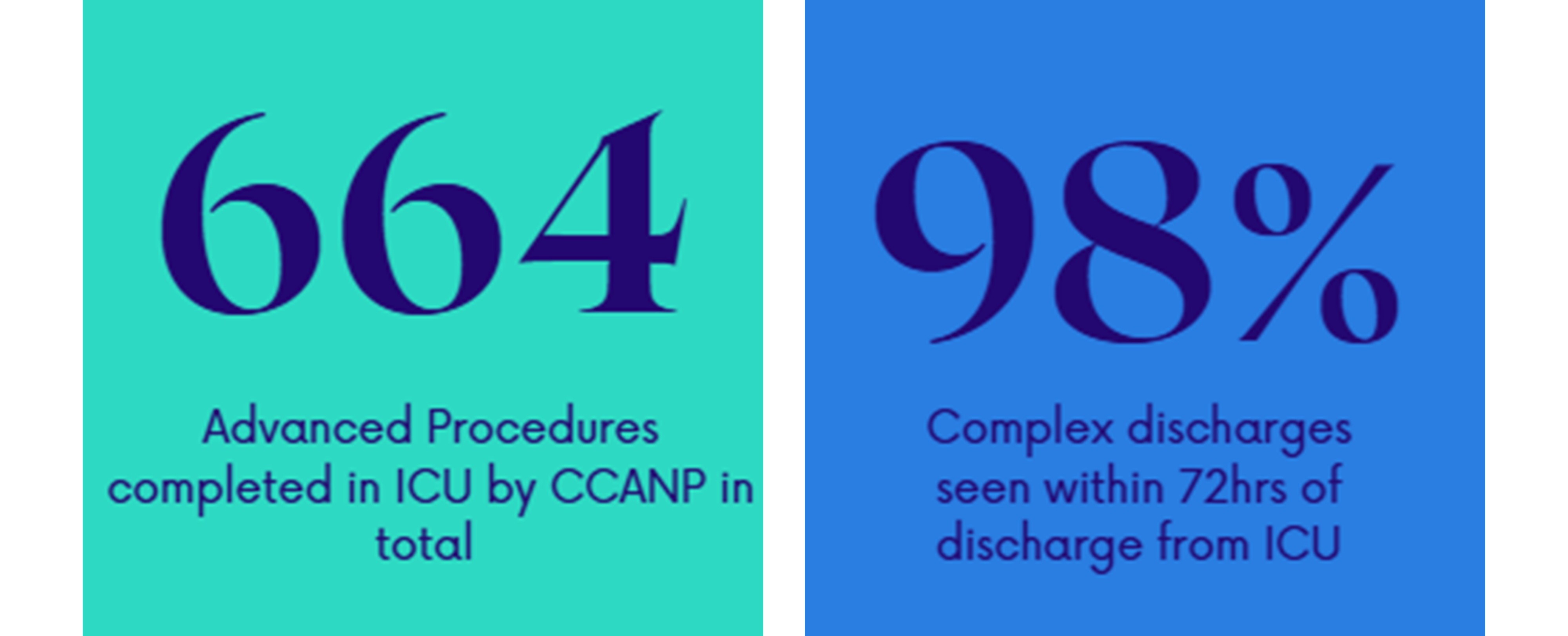
Enhancing the patient journey throughout ICU, the CCANP team lead manages a patient’s caseload and performs several advanced procedures. In 2024, 1,132 patients were reviewed by the CCANP team within the ICU and 664 advanced procedures were carried out including: arterial lines, male catheterisations, ultrasound guided vascular access and NG tubes.
The team also lead on several quality improvement (QI) initiatives. One of these is the ANP-led PICC line insertions service. This service means that patients can have specialised long term vascular access placed at their bedside in a timely manner without the need for transfer to the Interventional Radiology Department.
Another QI initiative the team are proud to lead on is the Antibiotic Allergy DE-labelling in ICU (ADE-ICU). Critically ill patients in ICU are frequently prescribed antibiotics, with many reporting an antibiotic allergy label, predominantly to penicillin. Mislabelling contributes to suboptimal antibiotic use, increasing multidrug-resistant organisms and Clostridium difficile infections, and increased hospital length of stay. Removing inaccurate labels decreases the risk of hospital acquired infections, e.g. MRSA, VRE, MDR-GNB, C. difficile and reduces hospital/ICU length of stay.
The ANP service in St James's Hospital aims to optimise the care and transition of the critically ill adult to and from the ICU. Recovery after critical illness can be a challenging journey for patients and their care providers. The transition from critical care to ward-level care is the first step in this journey, and patients are vulnerable to clinical deterioration and psychological distress.
The CCANP service aims to reduce errors, ease distress, identify risk of Post Intensive Care Syndrome (PICS) and optimise transition of care of the patient. In 2021, a traffic light system was developed by the CCANP and ICU consultant team to determine the necessity of post ICU review of patients on the ward. Red category patients were to be seen in-person, Amber category were reviewed at CCANP discretion and from Q4 2022, Green patients were reviewed remotely to identify TOC issues.
Another focus of our ICU stepdown reviews is to identify and support patients at risk of PICS. In 2024, 839 patients were followed up the team, 98% of all discharges from ICU. Over 70% of our patients are now surviving ICU, but survival often comes at a cost.

PICS is a relatively new concept which describes the sometimes-catastrophic impact of ICU survivorship on both patients and their families (PICS-F). PICS is made up of health problems that remains after critical illness. This led to the foundation of the ANP-led ICU Recovery Clinic. The ICU Recovery Clinic plays a pivotal role enabling patients and their families to understand their ICU journey and effectively manage symptoms of PICS. We hope that with this continued support from the CCANPs, our patients will not only survive but thrive as they adjust to life post-critical illness.
10-16 November marked International Advanced Nurse Practitioner Week. The theme of this year’s celebrations was “Trusted Voices, Proven Care”, and with over 1,380 ANPs nationwide, advanced practice nursing continues to play an integral and dynamic part in improving patient outcomes and the patient care experience. ANPs offer a valuable and cost-effective resource to address the challenges of accessible, safe and affordable health care.
The success of the CCANP role is in part attributable to and contingent on, the continued support of frontline staff nurses, Clinical Nurse Managers, Clinical Facilitators, medics and the wider multidisciplinary team across health and social care.